As much as beta amyloid is a hallmark of Alzheimer’s disease (AD) and widely believed to be involved in its development, many questions remain about this peptide and its connection to the development of cognitive decline and dementia. These questions are ever more pressing as numerous drug trials designed to remove amyloid from the brain have not shown that this halts or even slows the progression of the disease. Two CCNA researchers recently published studies in Nature Communications that provide important new insights about how these peptides develop in the brain and lead to cognitive decline, advancing our understanding of this complex neurodegenerative disease.
Abeta 34: a new piece in the Alzheimer’s disease puzzle
It has been known for a long time that beta amyloid is produced when the amyloid precursor protein (APP) is cleaved, or cut, by enzymes into smaller pieces, or peptides. These pieces vary in length between 30-51 amino acids. The most neurotoxic pieces, or species, have been found to be those that have 42 amino acids, referred to as Abeta (Aβ) 42. These also combine together to form into the sticky clumps called neuritic plaques that are found in the brain in Alzheimer’s disease. At the McGill Life Sciences Complex, the laboratory of Dr. Gerhard Multhaup (Professor and Chair, Department of Pharmacology & Therapeutics) has unlocked an important new finding. In their recent publication (“Aβ34 is a BACE1-derived intermediate associated with amyloid clearance and Alzheimer’s disease progression”, Nature Communications, 10:2240) the Multhaup lab details the linkage of an Abeta species they had discovered, Aβ34, to the development of AD. They determined that this peptide is created through the breaking down of Aβ 40 and 42 by into smaller non-toxic pieces by beta secretase 1 (BACE1), an enzyme generally associated with being involved in the cleavage of APP into Aβ 40 and 42 and amyloid buildup in the brain. The discovery of this new function of BACE1 suggests that efforts to inhibit its activity as a form of treatment for AD may not have worked because it reduced its beneficial as well as its negative effects. The paper also describes how (i) Aβ34 levels are elevated in individuals with mild cognitive impairment (MCI), a condition that often precedes AD, who later progressed to dementia, and (ii) Aβ34 levels correlate with the overall Aβ clearance rates in individuals with elevated Aβ levels. Moreover, compared to the gold standard Aβ40/Aβ42 ratio which is currently used by clinicians to help diagnose pre-symptomatic AD, a revised Aβ34/Aβ42 ratio may provide an earlier, more effective means to track the development of AD. Taken together, these findings suggest Aẞ34 could be an important element in earlier diagnosis of AD and in tracking the performance of potential treatments in the future.
Amyloid and cognitive decline: Not a direct relationship.
One of the most perplexing aspects of Alzheimer’s disease is that beta amyloid (Aβ) levels in some areas of the brain do not correlate well with the specific cognitive dysfunctions of people living with Alzheimer’s disease. In other words, the regions of the brain where AB levels accumulate do not correspond to the regions responsible for the cognitive functions affected. At the Douglas Research Centre, the laboratory of Dr. Pedro Rosa-Neto (Associate Professor and Director, McGill University Research Centre on Aging) addressed this apparent contradiction in their recent publication (“Aβ-induced vulnerability propagates via the brain’s default mode network”, Nature Communications, 10:2353). Dr. Rosa-Neto’s team determined that Aβ acts on cognitive decline in a two-step process. First, the accumulation Aβ in one region of the brain makes a second region vulnerable by decreasing its metabolism. Then, the presence of Aβ in this second region, combined with metabolic decline leads to cognitive dysfunctions. The regions where this process occurs in the brain are all part of the default mode network, a network of interacting brain regions associated with wakeful rest, thinking about others, self-reflection, remembering the past, and planning for the future. Dr. Rosa-Neto’s team first demonstrated this two-step process in humans and then replicated it in an animal model of Alzheimer’s disease. This is notable because there is a difference between the classic model of Alzheimer’s disease in humans and the animal model. In the animal model the accumulation of amyloid plaques is not accompanied by an accumulation of tau tangles (another protein associated with the disease), like it is in humans. This suggests that there is a neurodegeneration mechanism independent of the tau protein. These results indicate a new role for Aβ in cognitive decline and may represent a target for delaying or even stopping the progression of the disease.
These two important papers provide critical advances in our fundamental understanding of beta amyloid and ability to translate well-characterized basic science outcomes into improved clinical diagnostics and therapeutic strategies for AD. This gives hope that, despite recent setbacks, we may soon find more effective treatments for this devastating disease.
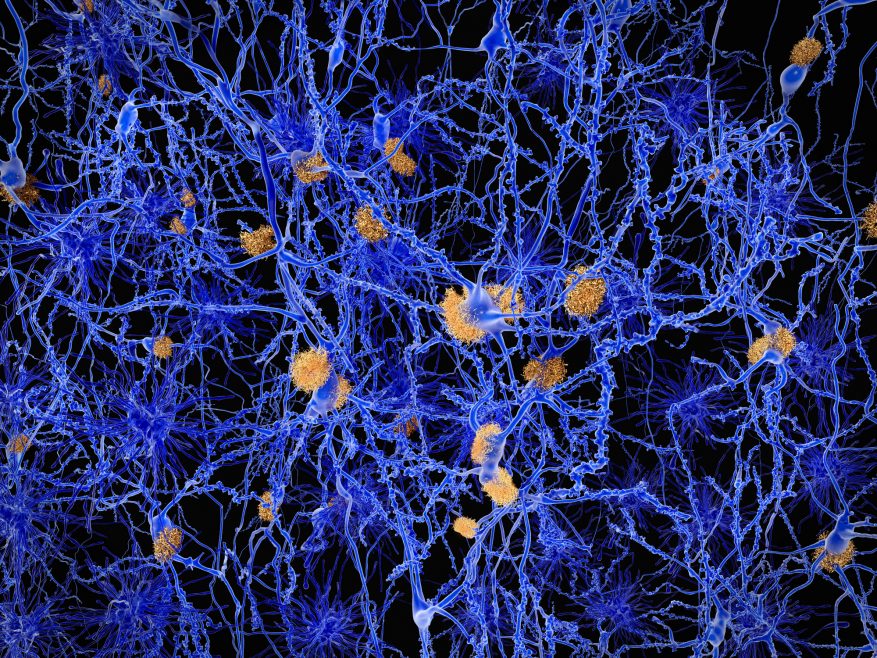
Featured image: Neurons with amyloid plaques. Amyloid plaques accumulate outside neurons and are characteristic features of Alzheimer’s disease. They lead to a degeneration of the affected neurons