
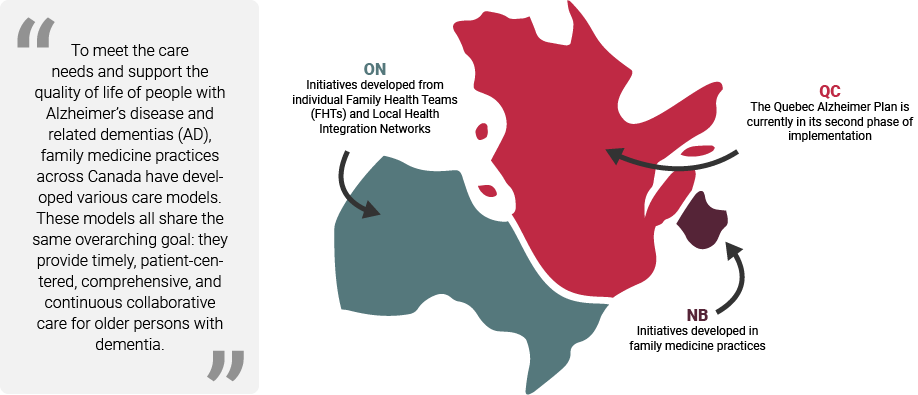
Assessing Care Models and Policies Implemented in Primary Health Care for Persons with Neurocognitive Disorders
To see how we evaluated these models and initiatives, see our research objectives and methods
Our work has long lasting impacts on clinicians, persons living with dementia and caregivers:
- Through several media interviews, articles appearing in the press and other lay publications we have contributed to general public awareness
View Media Section - We have engaged with clinicians to:
- Increase the knowledge and ability to care for people with dementia, especially in primary care.
- Make improvements in access, quality, and continuity of care for people with dementia.
- Facilitate collaboration between primary care clinicians and specialists around dementia care.
- We have influenced several provincial and federal policies when it comes to strategies for scaling-up initiatives across Canada:Our results were used by the Canadian Academy of Health Sciences (CAHS) during the panel requested by the Public Health Agency of Canada (PHAC) to examine the evidence available to support recent legislation creating a national strategy on dementia. These results continue to be used.
- The PHAC requested the CAHS to put together a report on available evidence 3 of our team members participated on the CAHS panel, plus results.
View the CAHS Report - PHAC continues to use our results in writing their national strategy on dementia.
- The PHAC requested the CAHS to put together a report on available evidence 3 of our team members participated on the CAHS panel, plus results.
Preliminary Results, News and Program Updates
Results:
Preliminary results in Quebec suggest that the Alzheimer Plan has had a beneficial impact on the quality of primary care for persons living with dementia and their caregivers. These results could be explained by the positive attitudes, practices, knowledge and competencies to detect, diagnose, treat and follow-up persons living with dementia in Family Medicine Groups.
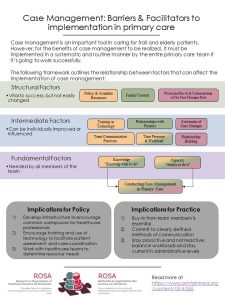
Finally, preliminary analyses suggest that the following elements must be present for the successful implementation of best practices: training and mentoring to clinicians; clinical tools; accompaniment by change managers; and identification of champions, case management mostly in the form of a dyad: physician-and-nurse. We have also been able to identify innovative practices that need to be scaled-up during phase 2.
Featured Results:
Dec ROSA KT |
|

|
|
|
 |
|
|
|
|
|
|
|
|
Executive Summary:
View the executive summary from our latest report to the Ministère du Santé et Services Sociaux du Québec (Quebec Ministry of Health).
English Executive SummaryFrench Executive Summary
Program Updates:
- 2016 newsletter
- 2017 newsletter
- 2018 newsletter
- 2019 newsletter
- 2020 newsletter
- 2021 newsletter
- 2022 newsletter
News:
To keep up-to-date on the latest news, follow @equipeROSAteam and check the #ROSAteam and #équipeROSA tags on Twitter!
06/07/2019PROVINCIAL COUNCIL STAKEHOLDER MEETING
Stakeholders from Quebec, Ontario, New Brunswick and Alberta, including decision-makers, managers, researchers, and patient and caregiver representatives, were invited to a meeting in Montreal, Canada on June 7th 2019. This full day meeting featured updates on the current state of the ROSA research program in Ontario, Quebec and New Brunswick, as well as on federal initiatives (Canadian Academy of Health Sciences report and Public Health Agency of Canada progress report on the Federal Dementia Strategy). Discussion centered around the use of interdisciplinary primary care teams, the integration of AD evaluation results into policy, and the use and accessibility of community services and resources.
View More Events
03/22/2019CCNA PHASE TWO FUNDING
Today, the Government of Canada announced the next phase of funding for the Canadian Consortium on Neurodegeneration in Aging (CCNA). From 2019 to 2024, CCNA will receive $46 million from the Canadian Institutes of Health Research (CIHR) and 11 other partner organizations, including the Alzheimer Society of Canada (ASC), and the Fonds de recherche du Québec – Santé (FRQS). Our research team ROSA (Research on Organization of Healthcare Services for Alzheimers), co-led by Drs. Howard Bergman and Isabelle Vedel continue investigating how to provide innovative care for persons living with dementia. Stay tuned as we unveil the new set of research objectives and methods in the coming months.
01/17/2019CAHS REPORT
Recognizing the importance of developing and implementing an effective strategy to address this challenge, the Minister of Health of Canada, through the Public Health Agency of Canada, asked the Canadian Academy of Health Sciences (CAHS) to provide an evidence-informed and authoritative assessment on the state of knowledge to help advance federal priorities under the National Strategy for Alzheimer’s Disease and Other Dementias Act.
To address the charge, the CAHS assembled a multidisciplinary, multi-sectoral panel of six experts with a range of expertise, experience, and demonstrated leadership in this domain, including several members of the ROSA team.
See More
Publication List and Media
Publications:
- Impact of the Quebec Alzheimer Plan on the detection and management of Alzheimer disease and other neurocognitive disorders in primary health care: a retrospective study
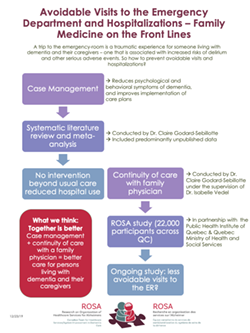
- Impact of health service interventions on acute hospital use in community-dwelling persons with dementia: A systematic literature review and meta-analysis
- Difference-in-differences analysis and the propensity score to estimate the impact of non-randomized primary care interventions.
Media:
- Watch Radio Canada’s mini-series on Alzheimer Disease, with Dr. Isabelle Vedel as a collaborator.
- Read a short opinion piece published by our team in The Gazette and La Presse on the need for multidisciplinary teams in treating AD
- See short videos of Claire Godard-Sebillotte’s (PhD candidate) research featured by CMAJ at NAPCRG and CCNA at their annual meeting
- Read a featured post on Nadia Sourial’s (PhD candidate) research
OUR TEAM
see the full ROSA team organigram
Principal Investigators:

Dr. Howard BergmanMcGill University |

Dr. Isabelle VedelMcGill University |
Co-Principal Investigators:

Susan BronskillInstitute for Clinical Evaluative Sciences |

Carrie McAineyUniversity of Waterloo |

Tibor SchusterMcGill University |

Yves CouturierUniversité de Sherbrooke |

Pam JarrettDalhousie University |

Shelley DoucetUniversity of New Brunswick |
|
|
|

Heather KellerUniversity of Waterloo |
|
|
|
|
The following page is authored by members of Team 19 of the Canadian Consortium on Neurodegeneration in Aging. Any questions regarding the content can be directed to: rosa-admin.fammed@Mcgill.ca








